oral surgery
‘operations in the treatment of disease or injury’
the word ‘surgery’ fills us all with dread.
reassuringly however, in the general dental practice setting oral surgery tends to be minor and relates mainly to the extraction of teeth, removal or drainage of soft tissue lesions, apicectomies, periodontal (gum) surgery, and implant placement.
tooth extraction
the vast majority of tooth removals are straightforward and pose no problems.
occasionally teeth may be impacted or difficult to remove because they are heavily diseased or restored.
impacted wisdom teeth
wisdom teeth are the last teeth to appear at the back of the mouth and often there is not enough room at the back of the jaw to accommodate them. they come through at an angle either pressing into the teeth in front or the bone behind and are difficult to keep clean.
pericoronitis
pericoronitis is inflammation of the soft tissues surrounding the crown of a partially erupted tooth, including the gingiva (gums) and the dental follicle.
it commonly occurs around the wisdom teeth at the back of the mouth and may settle down or come and go over a period of time.
if it recurs over and over, it is probably better to remove the tooth.
dental abscess
a tooth abscess is a pocket of pus that’s caused by a bacterial infection.
the abscess can occur at different regions of the tooth for different reasons.
a periapical abscess occurs at the tip of the root, whereas a periodontal abscess occurs in the gums at the side of a tooth root.
a periapical abscess usually occurs as a result of an untreated dental cavity, injury or previous dental work.
bacteria enter through either a dental cavity or a chip or crack in the tooth and spread down to the root and into the jawbone.
the bacterial infection can cause pain, facial swelling and difficulty eating.
treatment of the abscess involves draining it by way of incising the gum so reducing the size of the swelling, relieving the pressure and getting rid of the infection.
leaving a tooth abscess untreated can lead to serious, even life-threatening, complications.
apicectomy
an apicectomy is a surgical procedure to
- remove an infected tooth root tip
- clean out the surrounding infection
- place a filling to cap and seal off the new end of the tooth.
the most common reason to consider an apicectomy is persistent infection around a root tip, after conventional root canal work.
this infection can cause pain, swelling and discharge over the top of the tooth in the gum and can get quite extensive.
in some cases, it is preferable to repeat the root canal therapy, but this is not always possible or practical. surgery is then the best option to deal with the infection.
the suitability of apicectomy treatment can only be determined after thorough examination of the tooth’s appearance and x-rays/scans.
dental implants
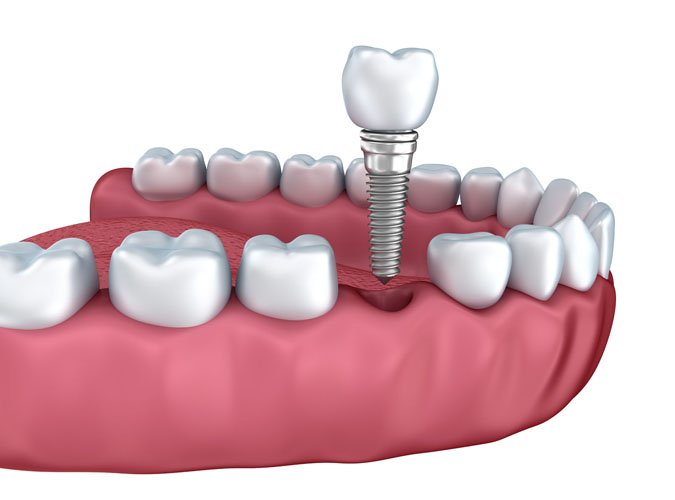
a dental implant (also known as an endosseous implant or fixture) is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor.
they are used to replace missing teeth. typically made of titanium, implants are screws that are placed into the jaw bone. the bone then grows into the threads of the screw and becomes ‘fixed’ i.e. implanted. the process is known as osseointegration.
within aseptic surroundings, bone is exposed in the jaw where the tooth is missing. the screw is inserted into the bone and the gum is stitched over it. it is then left for 3 months to allow the bone to integrate with it. if the integration is successful a second procedure is planned when the implant is exposed and the surface structure is made to fit the implant.
 not everyone is suited for dental implants.the gums must be healthy and there must be adequate depth and width of jawbone to house the titanium screw, although techniques are available to add additional bone if needed. dental hygiene must be excellent and maintenance i.e. regular dental visits are essential. general health is an important factor too, diabetics and smokers, for example, are not candidates for successful dental implant work as healing is diminished and the osseointegration less likely to occur.
not everyone is suited for dental implants.the gums must be healthy and there must be adequate depth and width of jawbone to house the titanium screw, although techniques are available to add additional bone if needed. dental hygiene must be excellent and maintenance i.e. regular dental visits are essential. general health is an important factor too, diabetics and smokers, for example, are not candidates for successful dental implant work as healing is diminished and the osseointegration less likely to occur.
the technology is however, very, very clever indeed. whilst implants are still no substitute for ‘real’ teeth, they certainly have improved the quality of life, in terms of eating, speaking and aesthetics, for many, many people.
tmj disorders
the joint between the upper and lower jaws, just in front of the ears is called the ‘temporomandibular joint’ – tmj. cartilage discs sit between this joint and the skull. if the discs slip or become worn, the tmj can cause problems. this is known as tmj dysfunction or tmj syndrome.
symptoms
all or any of the following;
- clicking when moving the jaw
- difficulty opening or closing the mouth
- swelling or tenderness in front of the ears
- pain in the neck, face or chewing muscles
- headaches or migraines especially in the morning
- earache
contributing factors
these vary from person to person. bruxism i.e. clenching or grinding the teeth when asleep or during the day. habits, for example biting your nails, chewing gum or pens. other factors include fatigue, stress and anxiety. underlying arthritis may also be a cause.
treatments
sleep clench inhibitors are often used to keep the teeth apart during sleep.
to ease symptoms it is advisable to cut food into small pieces, avoid chewy and hard foods, try not to open the mouth too wide e.g. in yawning.
professional treatments will try to focus on the cause of the problem, biteguards to restrict grinding, relaxation techniques, giving up aggravating habits, bite adjustment.
dental trauma
‘any trauma to the mouth that may cause bleeding and lacerations to the gums, and dislodge, or fracture teeth, and may require immediate medical attention’
if you have been in an accident and have had any sort of head injury, it is best to go to your nearest accident and emergency department. a traffic accident, falling of a bike, falling down stairs, or sustaining a sports injury can all cause an impact that breaks or loosens teeth, but your most serious injury could be concussion. you may need urgent assessment and observation to make sure that the accident has not caused any bleeding within your brain.
there are many different types of dental trauma, some of which have been highlighted here.
knocked-out (avulsed) tooth
this is one of the most serious dental traumas for permanent teeth. however, the damage can be fixed. if you act quickly, there’s a good chance the tooth can be saved.
when a tooth has been knocked out, the nerves, blood vessels and supporting tissues are damaged, too. the nerves and blood vessels can’t be repaired. that is why all avulsed teeth will need a root canal. however, the bone can reattach to the root of the tooth once it’s put back into place.
the odds of saving a tooth are highest in young children, but adult teeth can be saved as well. only permanent teeth should be re-implanted.
it is important to get to the dentist as quickly as possible after a tooth has been knocked out. it is also important to avoid damaging the tooth even more.
follow these suggestions to improve the chances of saving your tooth:
- handle the tooth carefully. try not to touch the root (the part of the tooth that was under the gum). it can be damaged easily.
- if the tooth is dirty, hold it by the upper part (the crown) and rinse it with milk. if you don’t have any milk, rinse it with water. don’t wipe it off with a washcloth, shirt or other fabric. this could damage the tooth.
- keep the tooth moist. drop it into a glass of milk. if you can’t do this, place the tooth in your mouth, between the cheek and gum. a young child may not be able to safely “store” the tooth in his or her mouth without swallowing it. instead, have the child spit into a cup. place the tooth in the cup with the saliva. If nothing else is available, place the tooth in a cup of water. the most important thing is to keep the tooth moist.
- try slipping the tooth back into its socket. in many cases, it will slip right in. make sure it’s facing the right way. don’t try to force it into the socket. if it doesn’t go back into place easily and without pressure, then just keep it moist (in milk, saliva or water) and get to the dentist as soon as you can.
displaced (extruded) teeth
this is a similar type of injury, usually caused by impact, but the tooth has not actually come out. It might have been knocked away from its usual position, or it might be hanging in by thin threads of tissue. after pushing the tooth back into position if you can, you need to see an emergency dentist as soon as possible, particularly if you are in a ‘hanging by the thread’ situation.
severe toothache
dental trauma relating to a blow to your mouth or jaw may result in severe pain in your teeth, there may be serious damage even though no teeth are obviously missing or broken. you will need an X-ray or other investigation to find out if you need treatment.
soft-tissue injuries
injuries to the soft tissues, which include the tongue, cheeks, gums, and lips, can result in bleeding. to control the bleeding, here’s what to do:
- rinse your mouth with a mild salt-water solution.
- use a moistened piece of gauze or tea bag to apply pressure to the bleeding site. Hold in place for 15 to 20 minutes.
- to both control bleeding and relieve pain, hold a cold compress to the outside of the mouth or cheek in the affected area for 5 to 10 minutes.
- if the bleeding doesn’t stop, see your dentist right away or go to a hospital emergency room. continue to apply pressure on the bleeding site with the gauze until you can be seen and treated.
periodontology
i.e the branch of dentistry concerned with the structures surrounding and supporting the teeth.
in layman’s terms, periodontology is the study and treatment of gum (periodontal) diseases. there are many different types of gum disease, the simplest and most common being gingivitis. the most complex, chronic periodontitis.
gingivitis
ie. inflammation of the gums.
it is said that 70% of the UK adult population has some form of gingivitis. in most cases it is a reaction to the build-up of plaque on the teeth and is non-destructive. the earliest sign of the disease is bleeding, commonly on brushing. they may also look red and swollen. this type of gingivitis is reversible. treatment involves improved oral hygiene and a professional scale and polish (hygiene visit) in most cases
chronic periodontitis
ie. inflammation of the tissue around the teeth, often causing shrinkage of the gums and loosening of the teeth
if left untreated, gingivitis will progress and the tissues holding the teeth in place will start to break down and detach from the teeth allowing more plaque build-up. this is called chronic periodontitis, also known as pyorrhoea. it involves progressive loss of the jaw bone around the teeth. although painless initially, if left untreated, it can lead to halitosis, abscesses and the loosening and subsequent loss of teeth.
treatment will require a periodontist (gum specialist) evaluation and may include tooth extraction and surgery. ideally, we’d like not to see anyone get to the latter stages of gum disease as treatment is more difficult and the outcome less predictable… as we would say…. ‘once a perio patient, always a perio patient’!!!
and the rest
there are a vast number of other types of gum disease. from types of acute gingivitis, gingival recession, stillman’s cleft etc. if you have a specific query, please give us a call and we’ll do our best to help.
